Modeling and Simulation of Cardiac Precision Medicine
In the Spanish health system there is an urgent need to focus on the millions of people with low prevalence and ultra-rare diseases, which are caused by mutations. Although genetic testing has improved the clinical management of cardiac disorders related to mutations, it is far from being solved, and arrhythmogenic cardiac events are continuously being reported. Arrhythmogeneity is also often attributed to pathologies such as atrial fibrillation, myocardial ischemia or heart failure. Atrial fibrillation (AF) is the most common arrhythmia, being responsible for stroke, thromboembolism, heart failure and tachycardia-induced cardiomyopathy. Heart failure (HF) is a common cardiovascular disease in which the heart muscle is unable to pump enough blood to meet the body’s requirements. This pathology is often accompanied by alterations in the cardiac conduction system such as left bundle branch block or right bundle branch block, leading to an asynchronous ventricular contraction and further reducing the left ventricular ejection fraction. Finally, myocardial acute ischemia is a life-threatening pathology that produces more than 7 million deaths worldwide. Most of these deaths correspond to sudden cardiac deaths related to lethal arrhythmias, especially ventricular fibrillation.
Precision medicine helps design personalized treatments, based on drug administration or on medical devices, to terminate these arrhythmias, however, the time and cost of the development of these therapies is very high.
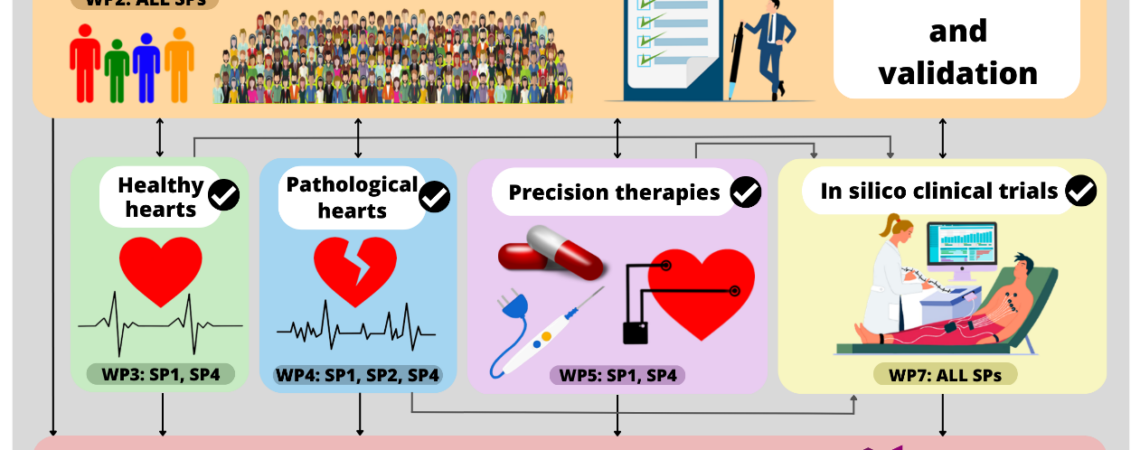
In this project precision medicine will be addressed to help in cardiac therapeutic research and development using modeling and simulation. Using clinical data provided by the clinicians in the consortium we will generate populations of electrophysiological and electromechanical cardiac models considering patient-specific characteristics, such as sex, anatomy, electrophysiology, and mechanics (in collaboration with subproject 4). Pathological conditions found in patients with genetic diseases, AF, MI, and HF will also be integrated. These models will be validated and tested in collaboration with clinical partners in subproject 3. We will also generate models of a wide range of therapies, such as drugs, ablation, and new approaches of resynchronization therapy, to perform in silico clinical trials and assess their efficacy. Cardiac safety of drugs will also be evaluated by means of in silico clinical trials in the presence of the cardiac pathologies considered in the project. In collaboration with subproject 2 new biomarkers will be defined, from clinical data and from the outcome of our simulations, which will be integrated into machine learning algorithms to better assess safety and efficacy, and risk stratification.
The members of this project are scientific leaders in cardiac modeling and have an ample experience in collaborating with clinical teams ensuring the success in the execution of the subproject. The results of the present in silico trials and precision medicine based on M&S will help in clinical guidance and diagnosis related to cardiac disease, and in reducing time and costs in the design of electrical devices or drug development for cardiac treatments.
Under execution